|
The HIMSS theme this year: "Health that Connects, Tech that Cares," highlights the importance of patient-centered practices that connect information, technology, and policy, emphasizing human-centeredness, quality, and interoperability. As forward-thinking tech companies proudly show off their achievements in chatGPT and generative AI, conservative healthcare providers are taking a more introspective attitude, assessing potential impacts and necessary responses. What breakthroughs can we expect at the intersection of these perspectives in the following years? Medical Coding and Payment in Digital Health Due to the pandemic, the U.S. has expanded digital healthcare payment coverage to include telemedicine, remote physiologic monitoring (RPM), remote therapeutic monitoring (RTM), remote assessments, and medical AI. In addition, Medicare is implementing a new Physician Fee Schedule (PFS) and influencing policies that promote medical quality and performance evaluation, such as the Traditional Merit-based Incentive Payment System (MIPS), the new MIPS Values Pathway (MVPs) framework, Alternative Payment Models (APMs), and Accountable Care Organizations (ACOs). As the industry focuses on digital, remote, and quality care, on-demand access to in-demand healthcare services is expected to create new business opportunities supported by more flexible and diverse coding and payment systems. Revenue Relates To Record Quality, Backed By Thorough Analysis And Documentation U.S. hospitals are struggling with prolonged revenue cycles, rising denial rates, and changing reimbursement regulations after the pandemic. To overcome financial challenges, many hospitals are turning to AI and analytics tools to improve the quality of medical records, address workforce shortages and burnout, and ensure both clinical and financial performance. Administrators, physician assistants, specialists, and clinical supervisors must collaborate in their clinical documentation integrity (CDI) efforts to capture missing data from various analyses. Traditional computer-assisted physician documentation (CAPD) systems are no longer sufficient; only proactive physician nudges and documentation assistance can effectively eliminate gaps in the medical record. For example, systems that flag hemoglobin or iron abnormality in lab data or identify brain lesions in scattered notes can actively remind physicians and expedite accurate diagnoses. While major vendors such as EPIC, 3M, and Optum offer these features, most are rule-based rather than AI-driven. Hospitals like Pediatrics still need to create their own rules and analyze data under the constraints of the system architecture to develop automated, customized nudge applications. Technology in Healthcare: Balancing Quality and Economic Benefits Speakers from UNC Health and Mayo Clinic revealed that their institutions have approximately 35,000-40,000 and 130,000 connected medical devices, respectively. Despite cybersecurity concerns, the medical data generated by these devices must be linked to medical records and utilized effectively. The vast amount of medical information can be standardized and coordinated only through analytics and AI tools that support medical record documentation, allowing healthcare professionals to access critical insights. Telemedicine policy has experienced profound reform in the wake of COVID-19. The recovering healthcare industry must adapt to the new digital era at its own pace. It may be too early for the widespread use of NLP and ChatGPT in clinical practice. Instead of blindly pursuing the latest technology trends, hospitals are more focused on adopting new approaches that effectively utilize various generations of technology to tackle both new and existing problems while balancing medical quality and economic benefits to improve patient outcomes and resource allocation. #himss23 #cdi Reference
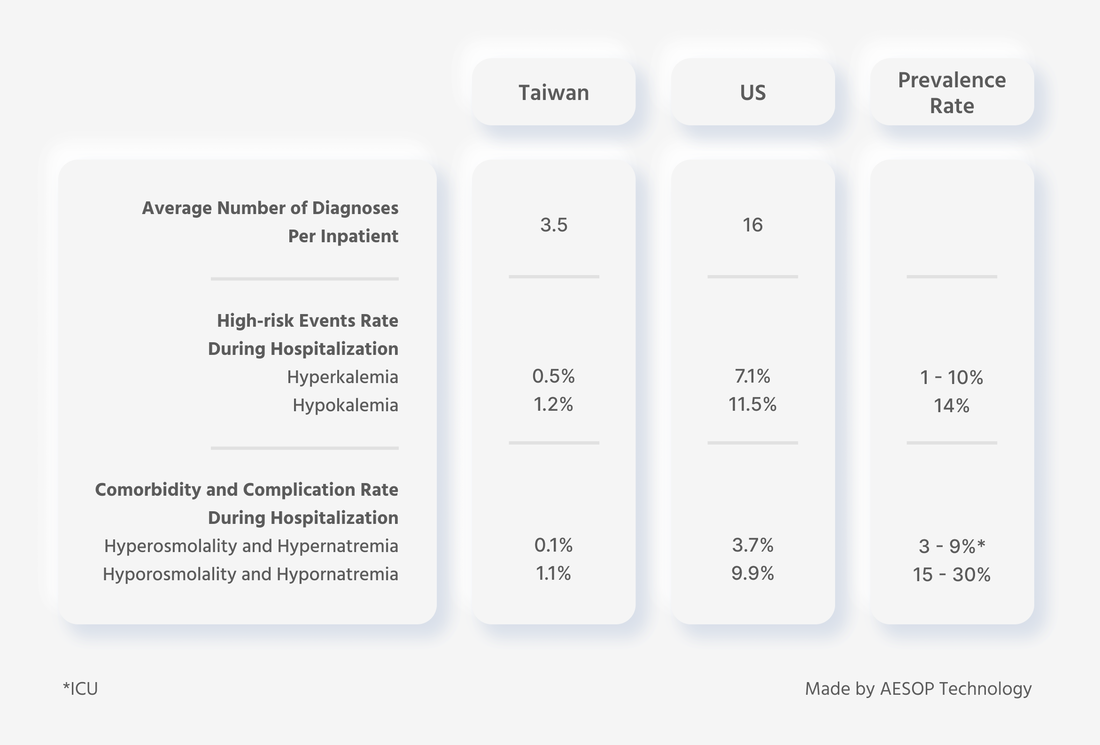
A comprehensive understanding of a patient's health status is important for effective treatment. This includes knowledge of their medical history, previous treatments and responses, recovery status, and any comorbidities that may impact treatment effectiveness. Accessing past medical records is the most reliable way to gather this information when a physician encounters a patient for the first time. However, the completeness of such documents cannot be guaranteed, and it is unclear who benefits from having complete records. It is often assumed that such administrative tasks are mainly for insurance purposes, but the importance of complete records extends far beyond insurance claims. According to a comparison of inpatient medical records in Taiwan and the United States conducted by AESOP's internal database, out of 20 million records, the average number of diagnoses per inpatient was 3.5 in Taiwan and 16 in the United States. Regarding high-risk hospitalization rates, the incidence rate of hyperkalemia was 0.5% in Taiwan and 7.1% in the United States. For hypokalemia, the incidence rate was 1.2% in Taiwan and 11.5% in the United States. As for comorbidity and complication rates, the incidence rate of hyperosmolality and hypernatremia was 0.1% in Taiwan and 3.7% in the United States, while the incidence rate of hyporosmolality and hypornatremia was 1.1% in Taiwan and 9.9% in the United States. In all three key indicators, Taiwan's data was lower than that of the United States, and even lower than the prevalence rate. Does this mean Taiwanese people are inherently healthier and less prone to severe illness? Our analysis revealed that Taiwanese people only appear to be healthier than Americans on paper, and this is because the healthcare reimbursement system in Taiwan provides fewer incentives for hospitals to record complete diagnoses, leading to an underestimation of the prevalence of various health issues. The All Patient Refined Disease Related Group (APR-DRG) system in the States emphasizes the severity of illness and risk of death. In addition, in recent years, the popular U.S. News & World Report hospital rankings have led hospitals to focus more on their rating categories, such as Elixhauser's Comorbidity Measure (commonly used in the U.S., while Taiwan uses the Charlson Comorbidity Index), 30-day post-discharge mortality rate, and 30-day readmission rate. These factors have significantly increased the incentive for U.S. hospitals to record complete diagnoses. Diagnostic completeness not only affects patient safety, healthcare reimbursement, continuity of care, and hospital revenue, but it also affects the truth of public health status and disease distribution. It has implications for future clinical research and development, healthcare budget allocation, and the effectiveness of related healthcare policies. However, collecting a complete medical record is challenging, especially in Taiwan, where comorbidity indices are rarely emphasized. The completeness of medical records can vary significantly between countries, and incentives for hospitals to record complete diagnoses can also differ in the same region. It is essential to emphasize the severity of illness, risk of death, and the accuracy of diagnoses to ensure patient safety, continuity of care, and effectiveness of healthcare policies. As diseases and information technology continue to evolve, it is essential to prioritize timely and accurate data inputting, efficient communication, and overall operational efficiency in medical record-keeping. Reducing the burden of post-hoc modifications on healthcare professionals will also be necessary to improve the quality and completeness of medical records. References It’s a familiar situation to many of us as patients. We met with our doctor, potentially about a severe problem, and during our consultation, they seemed distracted by their computer. Of course, in the past, doctors would write prescriptions on paper and write down notes to remember what we tell them, what they see, and what they hear from us during exams. But something seems different in this era of Electronic Health Record (EHR) systems. What is going on with those computers? Why do doctors sometimes seem frustrated with them? Why do they have to pay so much attention to them? Was it supposed to end up like this? As patients, we are not alone. Doctors can also be frustrated with what EHR systems have imposed on them. Even before COVID-19, physicians were struggling with burnout, and increased computerization of practice was cited as one of the major causes, often due to increased documentation demands. But why is that? EHRs: Easy on management, but pushing doctors to burnout One of the major reasons EHR systems are so challenging for physicians to use is that hospitals originally started to adopt them for accounting/financial and operation management purposes. Clinical treatment, or helping patients and clinical personnel, were all secondary considerations at best. A major feature of how they support hospital administration is by managing the processes they need to complete to be correctly reimbursed by insurance providers. This involves the enormously tricky problem of medical coding. Medical coding involves alphanumerically encoding each diagnosis, treatment prescription, medical action taken, and equipment used. The codes used are standardized and universal. It represents a continuous record of each patient's medical journey and is an essential reference for insurance providers. Medical coding is how providers can determine what diseases a given insured person has, how necessary treatment is, how complex it will be, what factors will affect treatment outcomes and more. Advancements in technology and knowledge, treatment techniques, disease classifications, and EHRs have also led to increasing complex medical coding systems. For example, there are now more than 68,000 diagnosis codes and 90,000 treatment codes that physicians need to consider when selecting the correct ones for a patient’s record. These codes are not something they need to know to treat patients, and memorizing the entire system would be a tremendous waste of time that they could spend on becoming a better doctor. For this reason high-quality medical coding can only be achieved by combining the experience and wisdom of doctors with that of coding experts that understand the insurance system. This involves the physician recording the diagnosis and treatment of the patient in their medical record. At the same time, coding experts are responsible for assigning corresponding codes to the diagnoses and treatments, using anatomy, physiology, treatment details, and healthcare reimbursement guidelines to ensure all the codes are correct from the perspective of the insurance system. So, rather than making life easier, EHRs have created new challenges for physicians. They need to work with medical coding experts and combine their expertise to complete the new task of creating sophisticated documentation that insurance companies can understand. This process can be exhausting. When a physician misses a diagnosis or inputs the wrong one, the coding team will “query” them to see if they can fix the patient record. Each query takes around 20 minutes to complete, in a context where physicians are seeing 10-20 patients a day, and the average number of diagnoses is over 50 per patient. Hospital coding improvements: Aiming to treat the root cause, but end up treating only the symptoms Let's look at the example of hospitalization due to a traffic accident. Within 72 hours after discharge, the doctor had to type in the diagnosis, treatment, and everything else from the patient's treatment process – only then could the all-important discharge record be generated. Based on their clinical experience and personal habits, the doctor listed the discharge diagnosis as "left lower leg crushing injury with necrosis." However, after entering the final diagnosis, this doctor faced a predicament: The system popped a warning stating, "No corresponding standard disease code found"! The doctor did a little more searching, showing 418 options for necrosis and 231 options for crushing injuries. The system also provided two seemingly identical options: "Excision of left lower leg subcutaneous tissue" and "Extraction of left lower leg subcutaneous tissue." While pondering all this, the doctor was also presented with a reminder from the hospital: "Maintain medical record quality! Maintain the balance between reimbursement and revenues!" And that's all just one case. As a medical professional, navigating the complex process of reviewing and coding medical records can be challenging while focusing on both clinical rationality and reimbursement. With a large volume of notes to review, doctors can quickly become overwhelmed and potentially lose sight of these necessary considerations. Doctors need to find balance, and a way to effectively manage this process to provide the best care for their patients while ensuring they are properly compensated for their services. Inevitably gaps between coding and the reality of the patient’s condition and treatments occur. Despite all this hard work, insurance billing problems, and documentation that can even affect healthcare quality downstream are still commonplace. Studies show that over 21% of US medical bills have diagnosis coding errors! CMS, the federal agency that runs the Medicare, Medicaid, and Children's Health Insurance Programs, also issued an alert in 2020 that federal healthcare insurance payments were wrong by as much as $900 million in the case of Medicare Part D, and a whopping $86.5 billion with Medicaid. Challenges physicians have with medical coding are a huge part of this. In the end, it results in devastating waste, abuse, and fraud in healthcare that causes a lose-lose situation for patients, hospitals, physicians, and taxpayers. Helping doctors focus on what matters To help doctors focus more on clinical practice, we at AESOP have developed DxPrime: a knowledge base constructed from 4.5 billion pieces of medical data, using machine learning to analyze inpatient and outpatient data from Taiwan and the US. Refining the combined wisdom of doctors and classification experts, we developed a proprietary model that utilizes AI multi-analysis to help doctors summarize discharge diagnoses. The system integrates directly into EHR systems and provides physicians with suggestions for discharge diagnosis packages by combining structural data from admission diagnoses, lists of multi-specialty questions, drug use, tests, exams, treatments, and surgeries. The doctor only needs to assess the diagnoses DxPrime presents to them to ensure clinical rationality, and choose one. DxPrime then automatically converts it into one of the built-in Diagnosis Related Groups (DRGs) that CMS and other insurance companies use to decide on the reimbursement amount. It drastically improves medical coding quality and costs, enhancing the reimbursement process and outcomes. This gives physicians more time to spend on what really matters, their patients. Medical AI needs to play a facilitator role in helping make up for human and systemic limitations. It will help doctors get insights from big data to create value in medical decision-making to achieve real data-driven clinical decision support. References 1. Medical billing errors growing, says Medical Billing Advocates of America 2. Billing Errors Everywhere! 3.2020 Estimated Improper Payment Rates for Centers for Medicare & Medicaid Services (CMS) Programs |
AESOP TalksExplore the intersection between healthcare and artificial intelligence.
All
|
|
AESOP TECHNOLOGY
|
 |
© AESOP Technology 2024