|
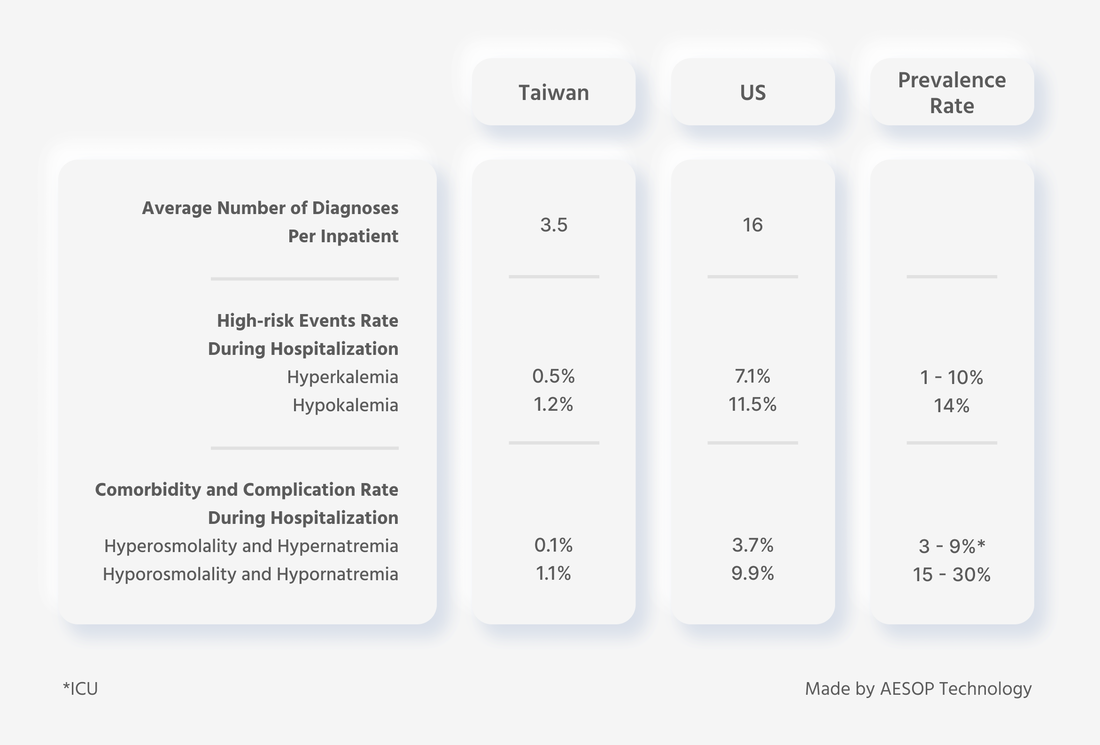
A comprehensive understanding of a patient's health status is important for effective treatment. This includes knowledge of their medical history, previous treatments and responses, recovery status, and any comorbidities that may impact treatment effectiveness. Accessing past medical records is the most reliable way to gather this information when a physician encounters a patient for the first time. However, the completeness of such documents cannot be guaranteed, and it is unclear who benefits from having complete records. It is often assumed that such administrative tasks are mainly for insurance purposes, but the importance of complete records extends far beyond insurance claims. According to a comparison of inpatient medical records in Taiwan and the United States conducted by AESOP's internal database, out of 20 million records, the average number of diagnoses per inpatient was 3.5 in Taiwan and 16 in the United States. Regarding high-risk hospitalization rates, the incidence rate of hyperkalemia was 0.5% in Taiwan and 7.1% in the United States. For hypokalemia, the incidence rate was 1.2% in Taiwan and 11.5% in the United States. As for comorbidity and complication rates, the incidence rate of hyperosmolality and hypernatremia was 0.1% in Taiwan and 3.7% in the United States, while the incidence rate of hyporosmolality and hypornatremia was 1.1% in Taiwan and 9.9% in the United States. In all three key indicators, Taiwan's data was lower than that of the United States, and even lower than the prevalence rate. Does this mean Taiwanese people are inherently healthier and less prone to severe illness? Our analysis revealed that Taiwanese people only appear to be healthier than Americans on paper, and this is because the healthcare reimbursement system in Taiwan provides fewer incentives for hospitals to record complete diagnoses, leading to an underestimation of the prevalence of various health issues. The All Patient Refined Disease Related Group (APR-DRG) system in the States emphasizes the severity of illness and risk of death. In addition, in recent years, the popular U.S. News & World Report hospital rankings have led hospitals to focus more on their rating categories, such as Elixhauser's Comorbidity Measure (commonly used in the U.S., while Taiwan uses the Charlson Comorbidity Index), 30-day post-discharge mortality rate, and 30-day readmission rate. These factors have significantly increased the incentive for U.S. hospitals to record complete diagnoses. Diagnostic completeness not only affects patient safety, healthcare reimbursement, continuity of care, and hospital revenue, but it also affects the truth of public health status and disease distribution. It has implications for future clinical research and development, healthcare budget allocation, and the effectiveness of related healthcare policies. However, collecting a complete medical record is challenging, especially in Taiwan, where comorbidity indices are rarely emphasized. The completeness of medical records can vary significantly between countries, and incentives for hospitals to record complete diagnoses can also differ in the same region. It is essential to emphasize the severity of illness, risk of death, and the accuracy of diagnoses to ensure patient safety, continuity of care, and effectiveness of healthcare policies. As diseases and information technology continue to evolve, it is essential to prioritize timely and accurate data inputting, efficient communication, and overall operational efficiency in medical record-keeping. Reducing the burden of post-hoc modifications on healthcare professionals will also be necessary to improve the quality and completeness of medical records. References Comments are closed.
|
AESOP TalksExplore the intersection between healthcare and artificial intelligence.
All
|
|
AESOP TECHNOLOGY
|
 |
© AESOP Technology 2024